Embryo transfer (ET)
ET is the final and most critical event in the success of an assisted reproduction cycle.
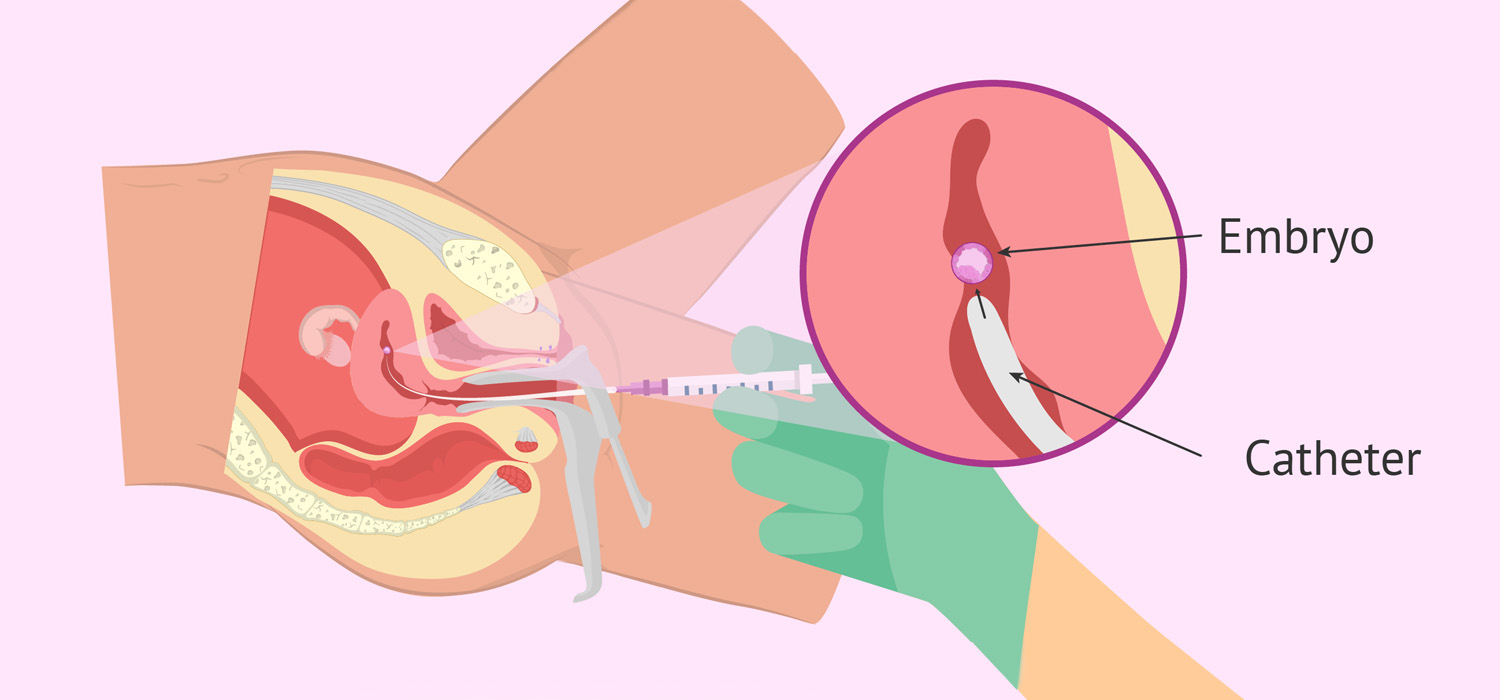
Definition: ET is the accurate and atraumatic deposition of embryos by means of an ET catheter into the uterine cavity, at an area with maximum implantation potential.
There is good evidence that atraumatic procedure, use of soft/ echogenic catheter, correct depth of transfer, ultrasound guidance and the experience of the clinician impact the implantation rates.
Types of embryo transfer
Transvaginal/ transcervical-Simplest, least invasive, and most widely used. However, this may not be feasible in cases of cervical stenosis.
Transvaginal/Trans myometrial- An 18G Towako ET catheter (Cook, Queensland, and Australia) with stylet is used. It is passed under ultrasound guidance through anterior fornix and anterior myometrium (Posterior fornix and posterior myometrium for retroverted uterus) stopping short of myoendometrial junction. Then after removal of stylet the preloaded inner catheter with embryo is threaded in and the embryos are released. This is performed when transcervical ET is extremely difficult and its disadvantage is that it can trigger myometrial contractions.
Sub endometrial embryo delivery-This involves using a hysteroscope for delivering the embryo into the uterus. Nitrogen, which is inert and non-embryotoxic, is used instead of carbon-di-oxide. This improves chances of implantation, prevents ectopic pregnancy, reduces inadvertent endometrial damage and the mils inflammation that it induces can favor implantation.
Steps of embryo transfer
The couple are counselled about the procedure, the number, stage, and grade of embryos available and informed decision is taken about ET/FET and the relevant forms are signed. The syringe and the inner catheter are flushed with the transfer media. The embryo/s are selected from the cleavage plate and serially passed through wells 1,2,3 to remove the oil and then loaded on to the catheter. After the outer catheter is inserted through the cervix under ultrasound guidance, the soft inner catheter with embryo (held horizontally with gloved hands in a cupped fashion to prevent exposure to cold air currents) is introduced through the outer catheter and the embryo is transferred. Catheter is kept in the uterus for 30-60 seconds and then slowly withdrawn, keeping pressure on the plunger of the syringe. Finally, the catheter is checked for any retained embryo before removing the outer catheter and the procedure is complete.
Factors affecting the success of embryo transfer
These include uterine cavity evaluation, uterine position, and mock transfer before ET; embryo quality; experience of the physician; use of uterine relaxants like progesterone; position of patient, physician’s preparation, and removal of cervical mucus during ET.
Embryo transfer catheters
An ideal catheter must be soft and flexible, non-embryotoxic, free of bacterial endotoxins, must be easily maneuverable and must be visible on ultrasound.
Commercially available catheters are soft or firm (rigid) ET catheters. Echogenic catheters offer better visualization due to ultrasonic contrast properties, minimizing the need for catheter movement to identify the embryo tip and hence shorter duration of ET. The amount of fluid volume has significant clinical impact, with volumes of 40-50 microliters reporting better PRs than 15-20 microliters.
Embryo transfer techniques
Preloading is when the embryos are already loaded on the catheter and given to the clinician at the start of procedure. After loading, the newer technique involves passing the empty catheter into the uterus and then the inner sheath loaded with embryo is threaded through the outer one. This also reduces the rate of difficult ET.
ET is performed under ultrasound guidance. Transvaginal/ transabdominal guidance yields the same pregnancy outcomes.
Transfer distance from the fundus (TDF) impacts pregnancy rates. The best rates are obtained when TDF is between 10-20 mms. Previous measurement of the length of endometrial cavity and cervical length go a long way in deciding and determining the place of ET.
It is advisable to transfer the embryos with the lowest possible speed as embryos exposed to fast ET had the slowest mean development rate and high apoptotic rates.
Et is likely to take longer in women with previous cesarean section and these also had a greater incidence of blood on catheter.
Tight temperature control throughout the ET improves clinical outcomes.
Difficult embryo transfer
There is no single definition of a difficult embryo transfer. An easy procedure with no additional instruments /maneuver is presumed to be an easy transfer.
Poor ultrasound visualization, touching the fundus, retained embryos, coiling of catheter inside the cavity, resistance to expulsion of embryos and presence of blood on catheter tip are all regarded as difficult transfers.
Post-embryo transfer
There is insufficient evidence to support any sufficient length of time women must be lying down after transfer. There is no evidence for adding fibrin sealants to the ET fluid either.
ASRM 2017 guideline recommendation
Grade A evidence:
- Transabdominal ultrasound guided ET improves CPR and LBR
- Use of soft ET catheters improves CPR.
- Bed rest after ET is not recommended.
Grade B evidence:
- Acupuncture does not increase LBR.
- Routine use of antibiotics is not recommended.
- Use of powdered gloves has no impact on pregnancy outcome.
- There is benefit in removing cervical mucus.
- ET catheter placement affects IR and PR.
- Immediate withdrawal of ET catheter is not recommended.
- The presence of mucus on ET catheter is not associated with lower CPR.
- Retained embryos in catheter and immediate retransfer do not affect PR.
For more info, Visit : www.medlineacademics.com