Endometriosis Aetiopathogenesis
Endometriosis is a condition where endometrial stroma and glands are present outside the endometrial cavity, causing chronic inflammation, with fibrosis. It is often a long term, debilitating, recurrent condition which poses a challenge for therapy.
It occurs in about 2-10% of the normal population, 20-50% of infertile couple and in over 60% of people with chronic pelvic pain and dysmenorrhoea.
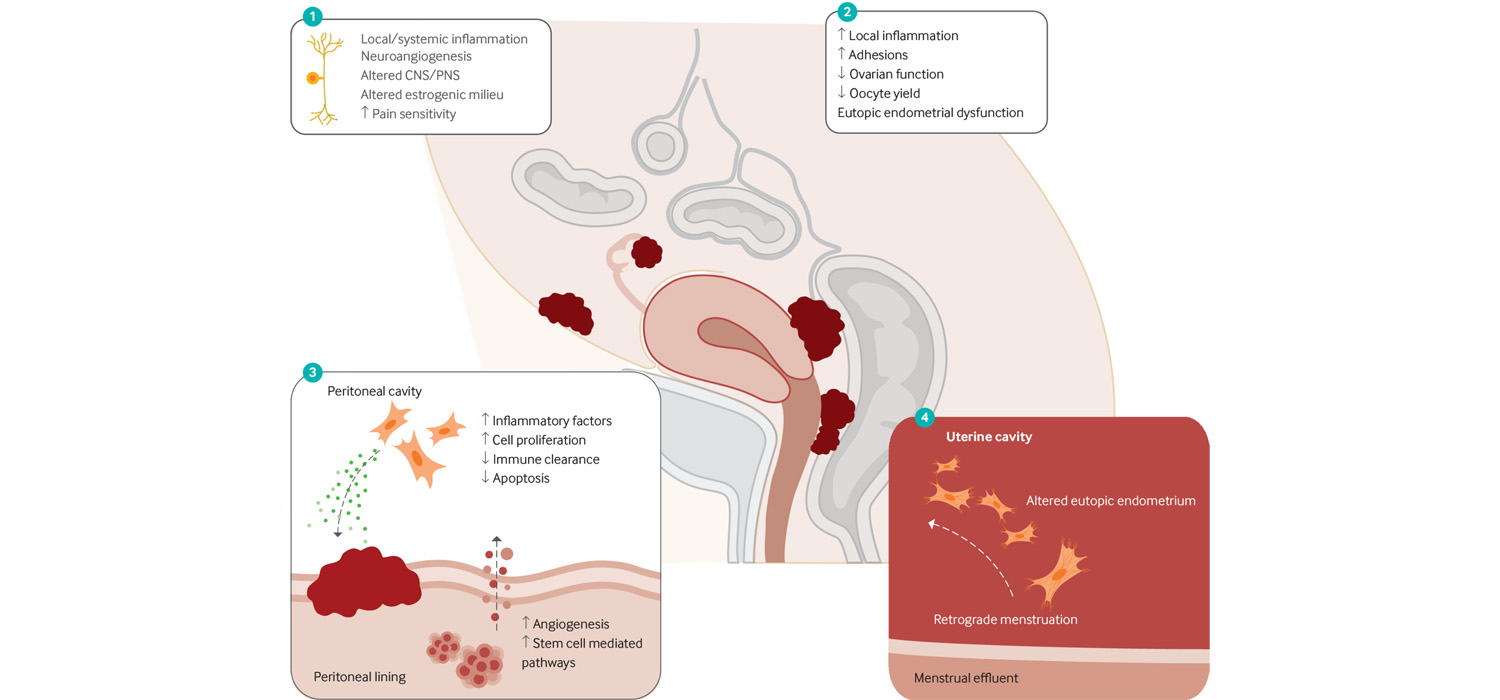
Pathogenesis of Endometriosis
Several theories have been proposed for the pathogenesis of endometriosis.
The Sampson theory of menstrual dissemination envisages retrograde menstruation from the endometrium via the fallopian tubes into the peritoneal cavity and over the ovaries.
The Coelomic metaplasia theory suggests that pelvic endometriosis may be derived through the metaplastic transformation of peritoneal mesothelium.
Vascular and/ or lymphatic spread of endometriotic tissue is another theory that aims to explain endometriosis at distant sites.
Induction of Mullerian embryonic rest cells not endometriotic activity is another theory. Bacterial contamination hypothesis that Escherichia coli infection of the genital tract causes endotoxin release into menstrual blood and then into peritoneum where an inflammatory response is elicited. because of with subsequent
Contributing factors include are genetic, hormonal influence (especially estrogen) and environmental insults like the endocrine disruptors.
Mechanisms causing fertility impairment in endometriosis
Endometriosis has ovulatory dysfunction due to several factors like abnormal folliculogenesis, poor oocyte quality, decreased fertilization rates, low-grade embryo formation, reduced implantation, luteal phase defects and luteinized unruptured follicle.
In Endometriosis, there is increased expression of xanthine oxidase which produces increased ROS (Reactive oxygen species). The macrophages, polymorphonuclear leukocytes in the peritoneal fluid, endometrial cells and apoptotic endometrioma cells all produce ROS. ROS causes oocyte damage, increased fragmentation at ICSI, DNA damage of oocyte, sperm, and embryo, thus adversely affecting the fertilization and implantation.
Increased amount of nitric oxide (NO) and nitric oxide synthetase (NOS) are seen in endometriosis. This has deleterious effects on tubal function and sperm motility and is toxic to embryos inhibiting implantation.
Endometriosis and sperm functions
ROS production by activated macrophages can induce DNA fragmentation, lipid peroxidation, in turn increasing membrane permeability and loss of membrane integrity. Severe Ros can also negatively affect acrosome reaction and sperm-oocyte fusion. The tubal ampulla binds with the sperms more tightly, reducing the number of free sperms available to fertilize the eggs.
Endometriosis and fertilization
Normally the follicular fluid (FF) induces acrosome reaction and binding of sperms to zona pellucida (ZP). But the peritoneal and follicular fluid in endometriosis inhibit the sperm-zona binding.
Endometriosis and implantation
Normally, during the WOI (Window of implantation) the cellular adhesion molecule αVβ3 integrin expression is increased. But this is decreased or absent in endometriosis resulting in reduced endometrial receptivity and implantation.
The adverse effects of endometriosis are seen even after conception and include deep placentation and predisposition to antepartum haemorrhage and pre-eclampsia.
Factors causing infertility in endometriosis
- Ovulatory dysfunction,
- Immunologic alterations,
- Peritoneal factors,
- Sperm inactivation and/ or phagocytosis by macrophages,
- Endometrial dysfunction interfering with implantation.
- Dyspareunia are some factors contributing to infertility.
- Anatomical distortion of tubes altered tubal motility, interference with ovum pick up and peri tubal adhesions are the mechanical factors that interfere with fertility.
For more info, Visit : www.medlineacademics.com