Male Genital Tuberculosis and Infertility
Tuberculosis (TB) is caused by Mycobacterium tuberculosis. The bacterium spreads through droplets when an infected person sneezes, coughs, etc. It primarily affects the lungs; however, it can spread to many other organs including male and female genitalia through blood, lymphatic drainage, or direct spread. Genitourinary tuberculosis is the second-most common extra-pulmonary tuberculosis.
Male Genital tuberculosis
Genital tuberculosis (GTB) is found in about 5-30% of genitourinary TB in men. GTB is mainly due to the primary reactivation of latent bacilli. In males, GTB can affect any part of the reproductive tract however the most common sites affected are epididymis and prostate. Isolated testicular TB is very rare due to the blood testis barrier and it comprises only 2-3 % of GTB. Similarly, TB of penis is very rare contributing only 1% of total cases of genitourinary TB. Involvement of the reproductive organs can result in infertility.
Route of spread
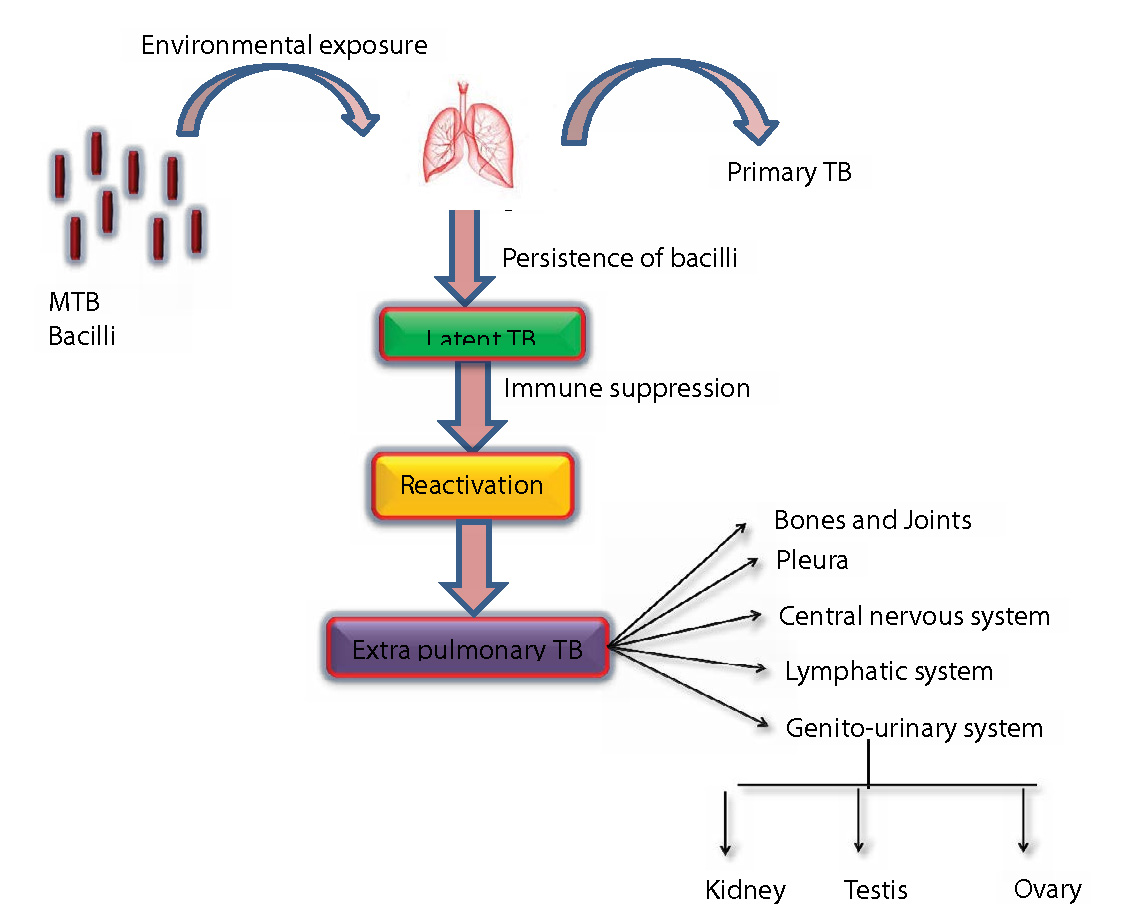
In Males, mode of involvement includes
- Secondary spread from infected urinary organs such as the kidney which then spreads to →Prostate, seminal vesicles, epididymis, and testis
- Hematogenous spread to epididymis or the prostate and primary reactivation of latent bacilli present in epididymis or the prostate
- The rest of the genital organs are involved by urinary/contagious/canalicular spread/lymphatic spread
- Penile TB (sexual contact with an infected partner/ reinoculation with a person's infected ejaculate)
Symptoms
Patients with genital TB can exhibit symptoms as follows
- Painless scrotal mass [can be painful in some] (bilateral involvement in 34%cases)
- Presence of abscess or a fistula (4-50%)
- Hydrocele (rare)
- Hemospermia
- Infertility
- Ulcerative penile lesion
On the contrary, some patients could be completely asymptomatic and diagnosed by incidental findings when presenting for other conditions.
Clinical finding:
- Semen analysis:
● azoospermia or severe oligospermia - scrotum:
● with or without tenderness
● With or without a draining sinus - Epididymis: Tender/non-tender nodules
- Prostate: nocturia, dysuria, hematuria, or Hemospermia. In neglected cases, there is development of a tubercular prostatic abscess or discharging perineal sinuses. Non-tender nodular prostate on rectal examination is also a finding.
- Penis: cutaneous lesions: single or multiple superficial necrotic ulcers. Cavernosal involvement destroys the glans penis/ erectile dysfunction.
- Urethra: urethral discharge in acute cases and strictures in chronic cases. Delayed cases can present with multiple discharging penile sinus/fistulas, recto urethra fistulas, etc.
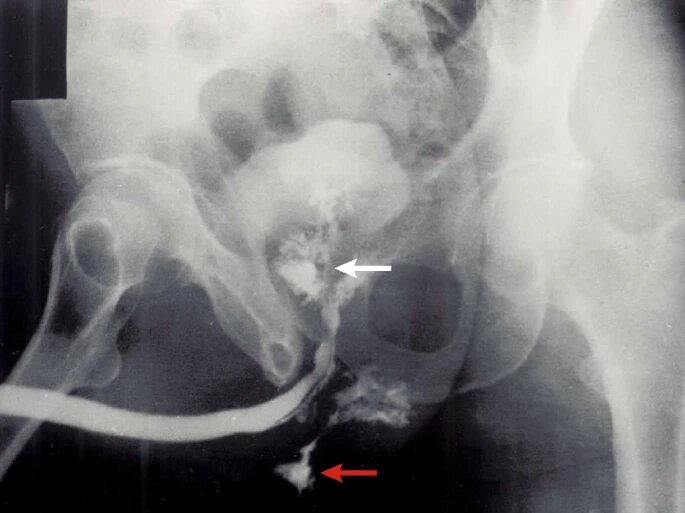
Diagnosis
Diagnosis is based on history and clinical findings and confirmed by the following
- Ultrasonographic findings provide supportive evidence
● Prostatitis- (multiple hypoechoic lesions in the peripheral zones along with calcification or abscess)
● Seminal vesiculitis- (enlarged and hypoechoic lesions)
● Epididymitis – (heterogenous hypoechoic diffuse or nodular enlargement of the epididymis with increased vascularity)
● Testicular abscess (hypoechoic lesion with sinus tract)
● extratesticular calcifications of the seminal vesicles, prostate, and the vas deferens - MRI: watermelon skin sign on the MRI suggests TB
- Ultrasound-guided fine needle aspiration cytology of the tissue: presence of epitheloid cell granulomas, multinucleated giant cell, and caseous necrosis.
- The gold standard criteria for diagnosis are isolation and culture of the mycobacterium tuberculosis bacilli from a clinical sample such as urine/semen/prostatic massage fluid/tissue/needle aspirates etc. One of the main advantages of liquid culture is that we can perform drug susceptibility tests and genotyping.
- Tissue PCR
- Urine microscopy and culture
- GeneXpert MTB/RIF assay – cassette-based analysis which gives results in 2 hours with the added advantage of identifying rifampicin resistance.
- Microscopy, culture, and PCR can be done on urine, semen, prostatic secretions, expressed prostatic secretion, post-massage urine, and post massage ejaculate may be useful.
How it causes infertility
Approximately 10% of patients with genital TB have infertility. Genital TB is destructive resulting in fibrosis and scarring, infertility arising from permanent damage to tissues can persist even after treatment.
Mechanism of infertility: Inflammation due to GTB→Obstruction of the terminal portion of the ejaculatory duct→leading to dilatation of vas deference→ Causes prevention of seminal vesicle secretions from reaching the ejaculate→ Azoospermia
Management of genital tuberculosis in male
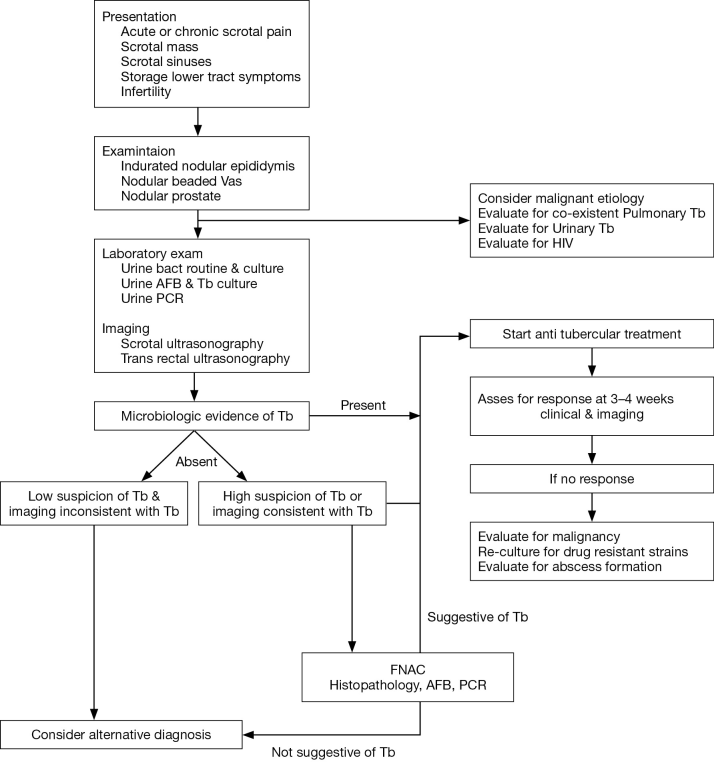
- Medical Treatment: Antitubercular treatment is the first line of management for genital tuberculosis. Medical treatment restores fertility in men who are in the early stages of infection when diagnosed. The drugs used are rifampicin, isoniazid, pyrazinamide and ethambutol. Longer duration of treatment may be needed for immunocompromised or HIV patients.
- Surgical treatment: Infertility per se results mainly from anatomic obstruction. Surgical management such as Open or percutaneous drainage of the abscess, etc is done for appropriate patients. Surgical treatment should be given after observing the response to initiation of chemotherapy for at least 4-6 weeks
- Treatment of infertility: most patients with genital tuberculosis will benefit from assisted reproduction. These men may be good candidates for IVF and their prognosis is similar to men with obstructive azoospermia.
Conclusion
Genital TB is an uncommon extrapulmonary manifestation of TB. In nearly 50% of patients with genital TB, there is a co-existing urinary tract involvement. Genital TB causes severe morbidity where damage can be irreversible. However, because of the vague symptoms, delay in diagnosis, anatomic distortion, and fibrosis, it is difficult to revert fertility even after treatment. Hence infertility arising due to genital TB is multifactorial and multifocal which in delayed stages does not benefit from surgical intervention also. However, testicular sperms are not affected, and these patients can opt for assisted reproduction with good overall success which is similar to non-genital tuberculosis patients.
To know more about etiopathogenesis and evaluation of male infertility enroll in our Basic Andrology course at Medline Academics. Get equipped with knowledge about advanced semen analysis techniques, cryopreservation, etc and become competent.