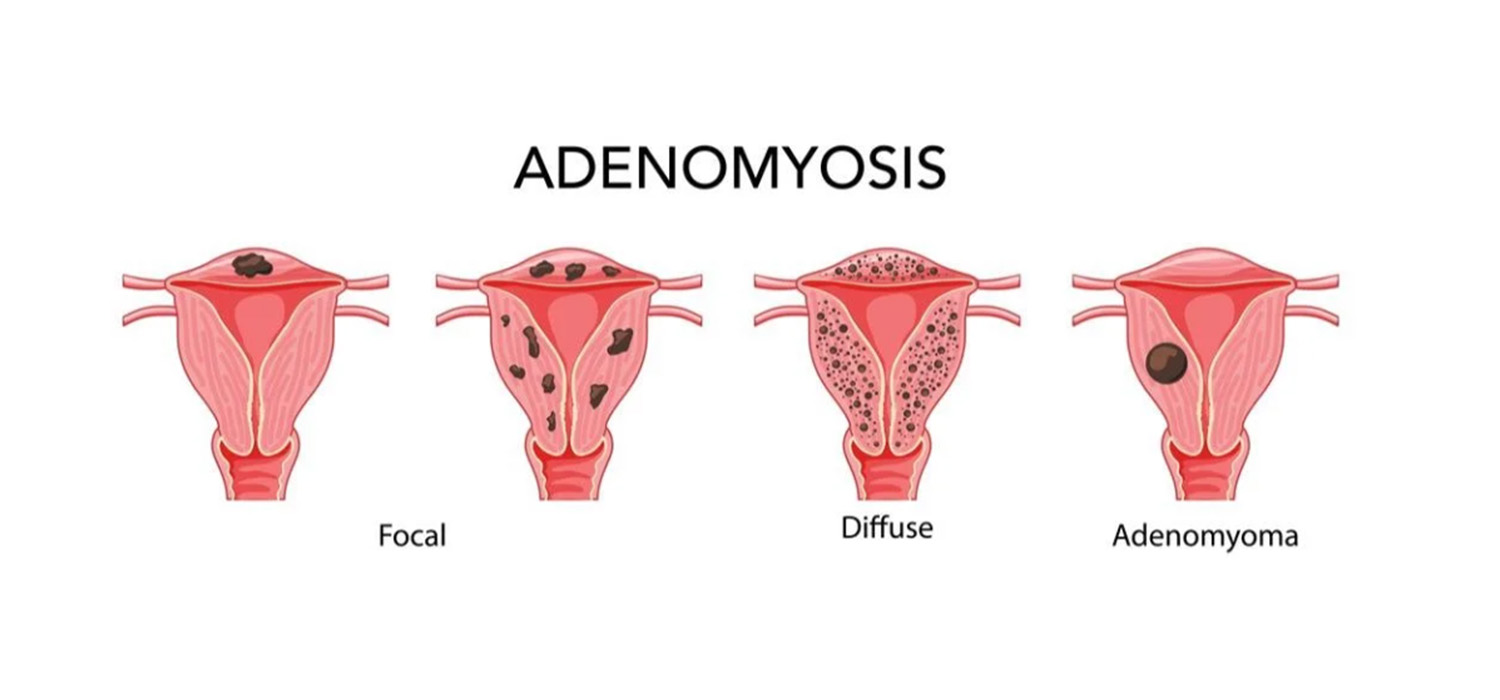
Uterine factors in infertility - Adenomyosis
Adenomyosis is the presence of endometrial glands and stroma within the myometrium. Symptoms of adenomyosis include dysmenorrhoea, menorrhagia, pelvic pain, and infertility.
Pathogenesis in adenomyosis
Polymorphisms in ER-Alpha gene have been implicated to increase the risk of endometriosis. Adenomyotic tissue has increased steroid receptors and increased aromatase and sulphatase activity. Estrone sulphate gets converted to estrone under the influence of the latter two enzymes. Estrone acts on the estrogen receptors within the tissue and causes further growth of adenomyotic tissue. Development and progression of adenomyotic tissue also reduces progesterone receptor expression.
What is the impact of adenomyosis on infertility?
Adenomyosis is associated with infertility and low success with ART. Reduced response to ovarian stimulation, reduced implantation, and clinical pregnancy rates, increased early pregnancy loss and reduced live birth rates in women undergoing IVF are some of the ways adenomyosis impacts fertility.
Investigations to detect adenomyosis
TVS and MRI can detect adenomyosis, the latter being more accurate in assessing JZ thickening and extent of myometrial involvement. HPE offers a definitive diagnosis.
Medical management of adenomyosis
Objective of medical management is pain relief, reduction in menstrual flow and to improve fertility.
The principle is to reduce the production of endogenous estrogen or to induce endometrial differentiation with progestins.
Non-hormonal agents are NSAIDs, pro-coagulants, Iron supplements. Hormones used for treating adenomyosis include progestins, combined oral contraceptive pills (COCPs), GnRH agonists (GnRHa)
Progestins cause decidualization and atrophy of the endometrium, modulation of mitotic activity, local growth factors and receptors; and affect the paracrine and anti-inflammatory mechanisms also.
Progestins
Nor-ethisterone acetate (NETa) in the dose of 5mg/day for 3 weeks on and one week off reduces bleeding and pain.
Danazol in doses of 200mgs/ day also reduces blood loss and uterine volume. It is not preferred because of its androgenic action causing deepening of voice and associated hypoestrogenic status.
Levonorgestrel Intrauterine System (LNG-IUS) that release LNG causes decidualization and atrophy of endometrium, downregulates the local estrogen receptors and thus reduces blood loss, pain, and uterine volume.
Dienogest is a highly selective progesterone receptor binding drug that inhibits cytokine secretion in endometrial stromal cells, inhibits cellular proliferation and induces apoptosis in the adenomyotic stromal cells.
GnRHa affects the adenomyotic tissue by inducing a hypoestrogenic state. Can be used in long stimulation protocols.
COCPs reduce aromatase expression, menstrual flow by causing decidualization and atrophy of endometrium.
Future therapies include Aromatase Inhibitors, SERMs and SPRMs. Further RCTs are needed.
Surgical management of adenomyosis
Surgery is beneficial for those with previous IVF failures, and it also increases spontaneous pregnancy rates.
Localised adenomyotic tissue can be excised by laparoscopy or robotic assisted surgical technique.
Sub-endometriotic adenomyotic lesions – within 2.5cms of endometrial surface can be managed by hysteroscopic resection followed by post-op estrogen replacement.
Diffuse adenomyosis may require prolonged treatment with GnRHa before ART but is associated with poor results.
ART for adenomyosis
Patients may be offered pooling cycles with FET. Pre-treatment with UPA for one or two courses, three months apart have been tried to improve results. However, further studies are needed. Surrogacy may be resorted to in cases of multiple failed IVFs.
Uterine Factor infertility due to Asherman’s syndrome
Intrauterine adhesions can occur secondary to pregnancy related curettage, infection of the uterus, post-surgery on the uterus and uterine tuberculosis which cause damage to the basal layer of endometrium.
Diagnosis is by HSG, ultrasound- 2D 7/or 3D, Sono-salpingogram and MRI. Hysteroscopy is the gold standard.
Treatment is indicated in those patients with infertility having hypomenorrhea and painful periods. Hysteroscopic resection of adhesions followed by IUCD insertion, estrogen therapy to prevent re-adhesions is the treatment offered. Endometrial regeneration using stem cells is being tried.
For more info, Visit : www.medlineacademics.com